Doctors are reporting high levels of COVID-19, flu and respiratory syncytial virus (RSV), as well as other “flu-like illnesses” that cause similar symptoms, such as the common cold, other coronaviruses, and parainfluenza viruses.

www.webmd.com
Virus Soup: Many Respiratory Viruses Peaking in Early 2024
Written by
Carolyn Crist
6 min read
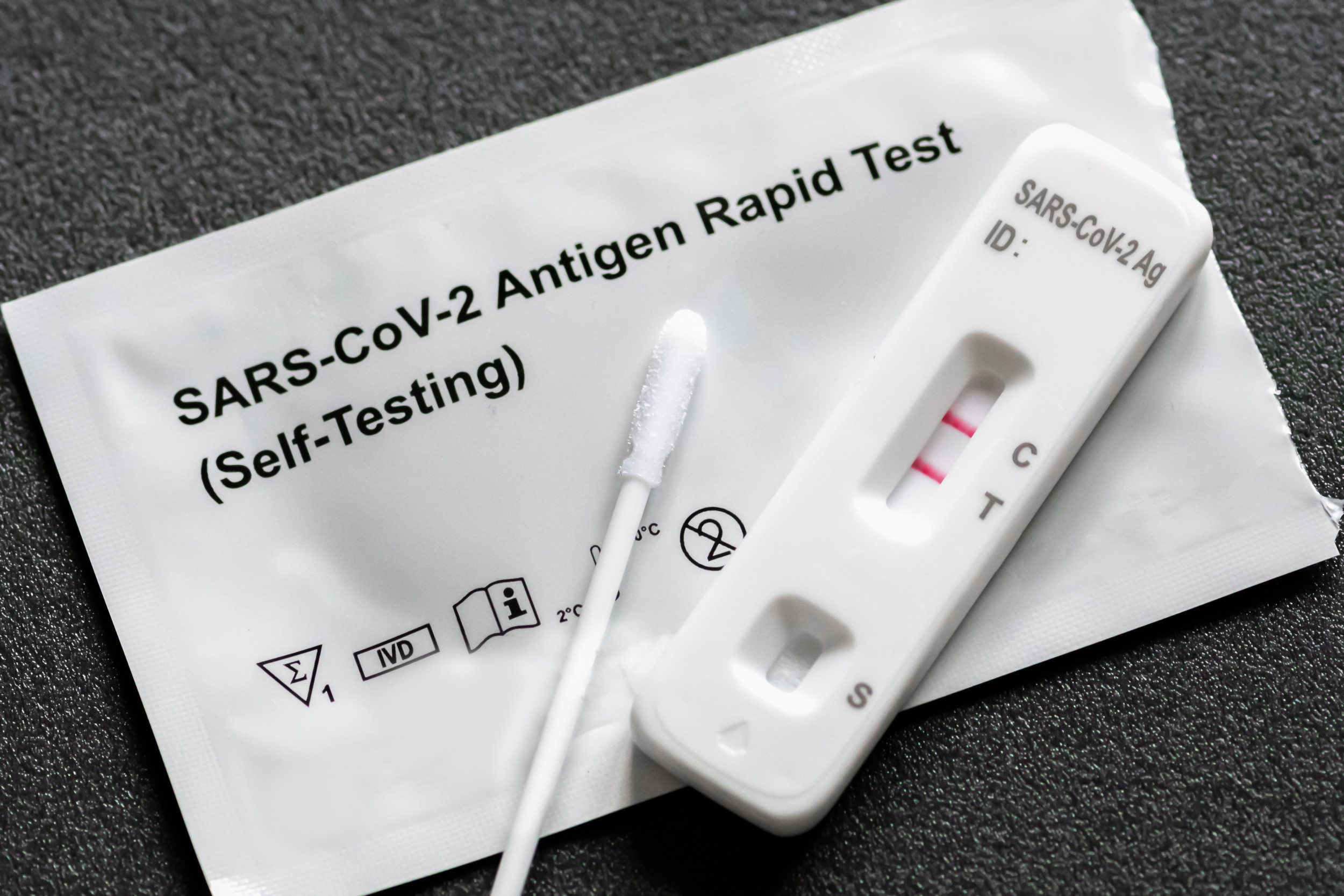
Jan. 19, 2024 – The familiar symptoms are back again – a runny nose, coughing, aches, congestion, and maybe a fever. When the at-home COVID-19 test comes back negative, you head to the doctor to see if they can figure out what you’ve caught. At the doctor, though, the typical COVID and flu tests also come back negative. It could seem like a new mysterious respiratory illness is making the rounds.
Instead, several typical respiratory viruses seem to be peaking at once. Doctors are reporting high levels of COVID, the flu, and respiratory syncytial virus (RSV), as well as other “flu-like illnesses” that cause similar symptoms, such as the common cold, other coronaviruses, and parainfluenza viruses (which cause typical respiratory symptoms such as a fever, runny nose, coughing, sneezing, and a sore throat).
“Respiratory viruses are still very high right now, as you would expect at this time of year,” said Brianne Barker, PhD, who researches viruses and the body’s immune response as an associate professor of biology at Drew University in New Jersey. “Also, a fair number of patients seem to have multiple infections at once, such as flu and strep, which may cause confusion when patients consider their symptoms.”
First-Aid Kit for Flu, Cold, and COVID-19
1/12
Pain Relievers
To help lower a fever and get some relief for uncomfortable body aches, be sure to have acetaminophen, naproxen, or ibuprofen on hand. However, if you have hypertension, kidney disease, or diabetes, you should be careful using NSAIDs. Aspirin also works, but don’t give it to kids. Aspirin is linked to a rare but life-threatening condition called Reye’s syndrome in children.
2/12
Other Meds
Decongestant nose sprays or drops with phenylephrine or pseudoephedrine as the active ingredient take down swelling in your nose and help you breathe better. Decongestant balms you rub on your chest can also help open airways. Cough medicines or drops with dextromethorphan help with a dry cough, while those with guaifenesin can soothe a wet cough.
3/12
Hand Sanitizer
For the best germ-killing power, wash your hands with soap and water whenever you can. But it’s a good idea to have a hand sanitizer with at least 60% alcohol around, too. Keep it by the bed when you’re sick, and use it after you cover a cough or blow your nose. Caregivers can grab a squirt, too, after checking a temperature or feeling a forehead.
4/12
Tissues
Coughs and runny noses can be features of colds, flu, and COVID-19. Keep tissues on hand so you can contain those germs that you’re hacking and sneezing. Use a tissue to cover coughs and sneezes. Throw tissues away promptly, and then wash or disinfect your hands.
5/12
Thermometer
Even if you’re not feeling feverish, it’s a good idea to track your temperature during an illness, so you have a good read on your body. You also need a thermometer in case your temperature spikes and you need to report it to a doctor.
6/12
Mask
It’s best to keep your distance from other people when you have a virus, but if you share a household or need to go to the doctor’s office, a mask that covers your nose and mouth is a must for keeping your germs to yourself.
7/12
Disinfectant Spray
The common cold, the flu, and COVID-19 are all airborne illnesses. That means they travel through droplets from your nose and mouth. When you’re sick, wipe down areas you touch so you lower the chances of passing the virus on to others.
8/12
Lots to Drink
Your body loses a lot of fluids when you’re sick because of fever sweats, a runny nose, and coughing. Water is good, but be sure to stock up on other kinds of drinks, too. Broth, warm tea, or drinks with electrolytes can all be good for hydration.
9/12
Humidifier
A cool-mist humidifier blows tiny droplets of water into the air to help keep your airways moist and ease stuffiness and dry coughing. Viruses are less likely to survive in humid air than in dry air, so it may help lessen the spread of your sickness, too.
10/12
Zinc Lozenges
While zinc lozenges won’t treat symptoms, studies show that if you start popping them at the first sign of cold or flu symptoms, they can cut the length of your illness by up to 40%.
11/12
Pulse Oximeter
A pulse oximeter is a small device that clips to your finger and reads how much oxygen is getting to your red blood cells. You don’t need one for a cold or the flu. But if you’re COVID-19-positive and having symptoms, it could help you keep tabs on how you’re doing. Normal oxygen levels are between 95% and 97%. Readings lower than that mean it’s time to call a doctor.
12/12
When to Go to Urgent Care
It’s important to know when your home remedies aren’t enough anymore. See a doctor right away if you or a loved one have trouble breathing, chest pain, confusion, trouble waking up, seizures, severe muscle pain, fever over 103 F, or aren’t peeing.
Next
Medically Reviewed by
Gabriela Pichardo, MD on November 18, 2022
So, what should you do? Wear a mask in public if you think you have symptoms, Barker said. Stay home if you feel sick, particularly if you have a fever over 100.4 F and signs of contagiousness, such as chills and muscle aches. Antiviral medications – such as Tamiflu for the flu and Paxlovid for COVID – may help if you catch it soon enough, but otherwise, it’s most important to stay hydrated and rest at home.
“The big picture is we’re in the heat of respiratory virus season, and the big player at the hospital right now is the flu, which seems to be superseding everything else,” said Dhaval Desai, MD, director of hospital medicine at Emory Saint Joseph’s Hospital in Atlanta. “I’m not sure if certain viruses are more aggressive or different this year, so it’s hard to say exactly what’s going on, but we’ve certainly seen an uptick since mid-December, and it hasn’t stopped.”
What Are the Latest Trends?
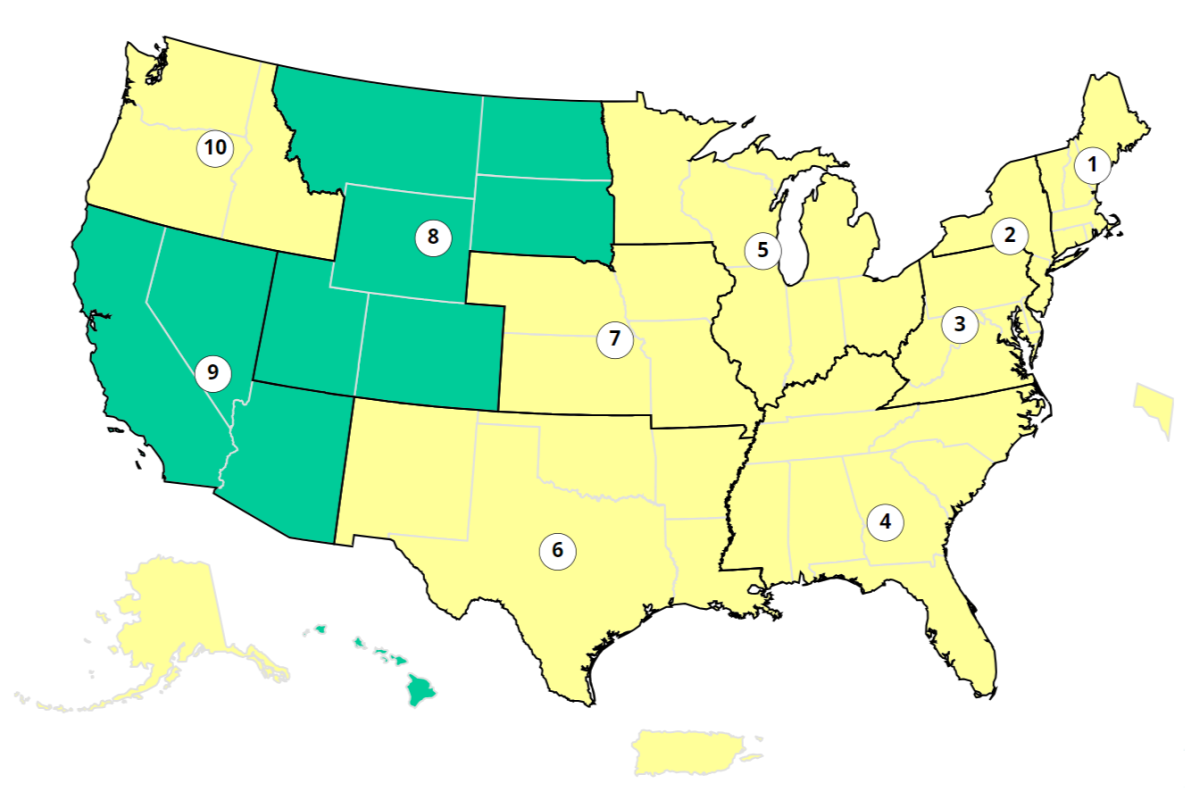
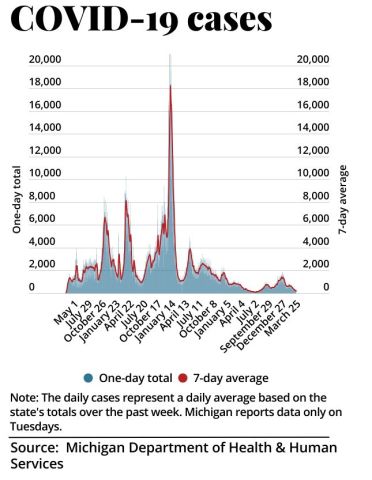
The current COVID-19 surge appears to be at the highest point since the Omicron variant infected millions in December 2022, according to the
CDC's COVID wastewater data. Test positivity appears to be stabilizing after increasing since November, the CDC’s
COVID Data Tracker shows, though the rate was still high at 12.7% positivity during the first week of January.
At that time, COVID-19 emergency department visits began declining, though hospitalizations were still on the rise and deaths were up 14.3% from the previous week. As of Jan. 6, the JN.1 variant is driving most of the spread, accounting for 61.6% of COVID-19 cases in the U.S., according to
CDC variant data.
“COVID doesn’t seem as bad right now as in the days of Omicron, but the problem is that it’s tough to compare because COVID cases aren’t reported in the same way as before, and we don’t have that state data,” said Bernard Camins, MD, an infectious disease specialist and medical director of infection prevention at Mount Sinai Health System in New York City.
The good news, he said, is that hospitalization rates are lower than last year, considering the number of people getting infected, “so there’s some immunity to it now.”
“The other good news is we have treatments for COVID, such as Paxlovid, that most people can take as long as they talk to their doctor as soon as possible after they get infected.”
00:0000:00
ABOUT TRANSCRIPT
Cold vs. Flu
Cold and flu viruses share certain symptoms. Here’s how to tell the difference.
Influenza rates, which dropped during the height of the COVID pandemic, appear to be back at typical levels, Camins said. This flu season started earlier than usual in 2023 and will likely peak in the next few weeks. The
CDC’s FluView shows that test positivity – now at 14% – is increasing, and hospitalizations and deaths are trending upward as well.
Similarly, the CDC’s
national trends data for RSV shows that cases rose as high as last year’s peak in recent weeks but appear to be declining now, especially in the Northeast and South.
Other viruses are circulating as well, such as adenovirus, which can cause a cold, sore throat, diarrhea, pinkeye, and other symptoms. Parainfluenza viruses peaked in late November and saw another jump at the end of December. Rhinoviruses, which cause the common cold, also returned to normal peak levels alongside the flu this season, Camins said.
“I haven’t gotten sick since 2021 and recently got rhinovirus, and it went through my household. The symptoms weren’t severe, but I still have a lingering cough,” he said. “The trick is that people weren’t getting exposed in previous years due to masking and other precautions, but now people are getting exposed to many of these viruses.”
What Should We Expect Next?
Peak respiratory virus season will likely continue throughout January and February and then begin to fade as the weather warms up, allowing for outdoor activities, better ventilation, and higher humidity.
“One of the reasons why we see so many infections at this time of year is related to humidity, when the respiratory droplets containing these viruses stay in the air longer and the immune response in our nose actually works less well in dry air,” Barker said. “Evidence indicates that having increases in humidity can help get rid of some of the viruses in the air and help our immune response.”
In the meantime, Barker suggests taking precautions, stocking up on at-home tests, and staying home when you're sick. She recently recovered from an upper respiratory infection and has decided to wear a mask in public places again. She tested negative on every possible test at her doctor’s office and doesn’t want to repeat the experience.
“It reminded me how much I don’t enjoy having an infection,” she said. “I’m willing to wear a mask at the grocery store if I don’t have to go through that again. I’m taking care of myself and others.”
In addition, don’t hesitate to get tested, Desai said, especially if an antiviral could help. After getting a respiratory virus in November, he had a high fever and sweating and decided to go to his doctor. He tested positive for influenza A, or H1N1, which the CDC’s FluView says was the most frequently reported flu strain at the end of December.
“It kicked me harder than other illnesses in recent years, but I did take antivirals, and it was out the door in about 4 days,” he said. “My mom, who is immunocompromised and in her 70s, also got it but took an antiviral even sooner and got over it in about 24-36 hours.”
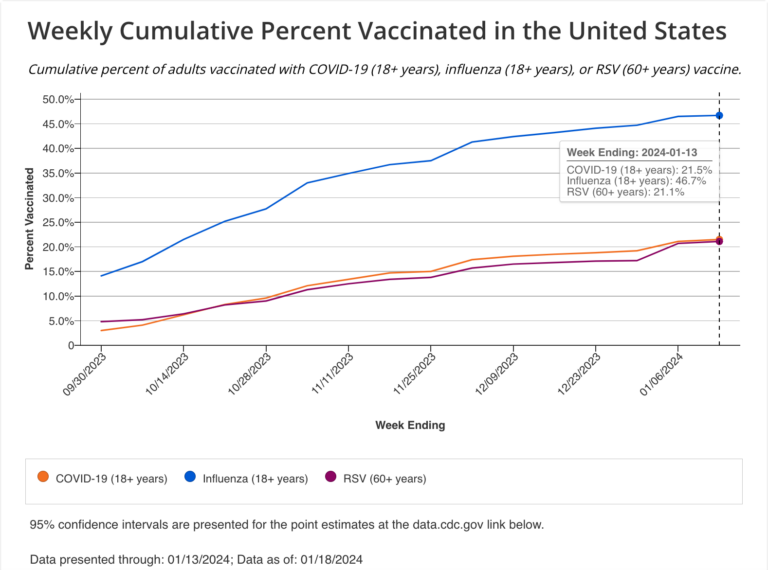
For the next couple of months, it’s also not too late to get vaccinated against the most prevalent viruses, especially COVID, the flu, and RSV. The most vulnerable groups, such as young children and older adults, could especially benefit from vaccination, Camins said.
“With RSV, for instance, there are vaccines for pregnant women to protect their infants,” he said. “And although we don’t have great data to say whether the current COVID vaccine is protective against infection, we know it still protects against severe disease and death.”
As 2024 continues, experts said they’re looking forward to more effective at-home tests for COVID and the flu, better flu vaccines, and new research on the body’s immune response to these respiratory viruses.
“Disease prevention is key, irrespective of what’s surging and what we’re dealing with right now,” Desai said. “Think about your risk factors and what you’re doing overall this year for your health and wellness – whether routine physical exams or cancer screenings, based on your age. There’s power in staying healthy and advocating for ourselves when we’re feeling well.”









 Alexia Aston
Alexia Aston