Your Antibiotic is Sick: Bacteria are defying the most powerful medicines of all time. Is India ready for a world without antibiotics?
The patient is going into shock. His blood pressure is falling. Antibiotics don't seem to work. "Dr Sumit Ray sprinted to the intensive care unit in response to the urgent call. He had dreaded this moment ever since the 22-year-old car crash victim was admitted to Sir Ganga Ram Hospital, Delhi: His blood culture, done on admission, had detected bacteria specimens resistant to a range of antibiotics. Over the last five days, his head injury had healed but a spiking fever had appeared, suggesting infection. Through the glass wall, Ray, vice-chairman of critical care at the hospital, could see the ashen pallor that made the patient's face blend with the sheet. "He's sliding into a septic crisis. Soon, the infection will turn unstoppable," he sighed.
Who can tell what germ is hiding in one's body, awaiting its chance to create havoc? A nagging fever that spikes to 103 degree celsius. Painful rashes that turn into pus-filled pockets. Black, bloody or tarry stool that just won't clear up. Swollen glands that look angry and enlarged. You know your antibiotic is not working if within 24-48 hours your body gives tell-tale signals of germs outsmarting drugs. If you don't pay heed, they will invade your bloodstream, driving you into a life-threatening crisis. Sounds like a science fiction nightmare but it's more real than you might think.
Armed with antibiotics, 'miracle' drugs of the modern era, doctors today know practically no limits to the range of patients they can help. All that progress is suddenly being challenged by invisible legions of malevolent bacteria, one millionth of a milli-metre in size. Hospitals are turning into hotbeds of infection. And the drug development pipeline for new antibiotics is running dry the world over. India is in a particularly tight spot. Union Health Minister Ghulam Nabi Azad has faced fierce questioning during the current Budget Session of Parliament on the rising tide of antibiotic resistance (ABR) in the country. An urgent question hangs over the future: What if antibiotics do not work anymore?
The World Health Organization (who) has raised alarm on the "serious, growing, and global threat" since 2010. At the 2013 World Economic Forum (WEF) at Davos in January, who Director General Margaret Chan warned that bacteria are becoming so resistant to common antibiotics that it could mean "the end of modern medicine as we know it". With ABR snuffing out 100,000 lives in America, 80,000 in China and 25,000 in Europe a year on average, wef considers it "one of the chief threats to human health" that the world is "mostly unprepared to cope with".
Smart guys of evolution
Alexander Fleming had cautioned even on the day he received the Nobel Prize for discovering penicillin in 1945 that antibiotics would lead to a bacterial backlash. In the history of life, bacteria are the smartest: They double in numbers every 20 minutes, with each bacterium creating 16 third-generation progeny in an hour. Every generation passes on to the next the genes essential for survival in a hostile atmosphere. "Antibiotics are tiny molecules that enter into bacteria cells to destroy them," says Sarala Balachandran, chief scientist with the Council of Scientific and Industrial Research (CSIR). "To protect themselves, bacteria mutate their genetic make-up." They multiply rapidly, passing on resistant genes to new generations. It's the Darwinian principle of natural selection. "If you don't finish a course of antibiotics, not all bacteria die and you are likely to get the resistant strains."
Dimple Kumar, 20, of Patna nearly paid with her life for that one irresponsible habit: Not completing courses. It did not matter until she got blisters at her waist from tying salwars too tight, which caused an infection. For six months, doctors kept raising the antibiotic doses, but the infection continued to spread deep inside her tissues. She landed up in a hospital with pus-filled sores, swelling, high fever and falling blood pressure. After four surgeries in four weeks, a last resort antibiotic finally worked on her. "I was lucky. I could have died," she says.
50 per cent antibiotics are overused and misused by physicians and patients globally.
70 per cent ICU patients surveyed in India carry bacteria immune to multiple antibiotics.
30 per centinfants die in India each year from germs that do not respond to antibiotics.
95 per cent rise in pneumonia, blood and wound infections in last 10 years in India; can’t be cured by last-resort drugs.
The hidden epidemic
It was a deadly bacterial gene with a tongue-twisting name, New Delhi metallo-beta-lactamase (NDM-1), that brought ABR first to public attention in 2010. Chennai microbiologist Karthikeyan Kumarasamy caused a medical uproar when, along with British researchers, he first reported in Lancet Infectious Diseases that NDM-1 infections were found in patients returning from India after medical treatment. NDM-1 makes a bacteria resistant to all known antibiotic-even carbapenem, known as the last resort. That unleashed a veritable war of words. The naming of the bug after Delhi was seen as an insult and the report was rubbished as an "alarmist" and "motivated" attack on India's booming medical tourism industry. "It's a growing menace," says Kumarasamy. "The Government should initiate a national survey and then institute an antibiotic policy. But nobody is listening."
The hidden epidemic is upon us, says health economist Ramanan Laxminarayan, director of the Washington-based Center for Disease Dynamics, Economics & Policy (CDDEP). He has been preparing economic models of ABR for the last 16 years. "You must have noticed doctors now give longer courses and that antibiotics are becoming more expensive. That shows ABR is rising," he says. He entered the new field of "resistance economics" in 1996, fascinated by the stories he heard from his teachers. "Say, how the excessive use of penicillin on Vietnamese sex workers by US military troops to prevent gonorrhea made it totally resistant." But it was not until 10 years later that he started meeting people with ABR from simple injuries. "It has grown exponentially in the last 5-6 years. We are on a steep curve."
A sign of the time: One million infants die in the first four weeks of life every year in India. Over 190,000 deaths occur due to bacteria in the blood. And 30 per cent of babies die of ABR, reports cddep. "Neonates stay in the sterile and safe atmosphere of the mother's womb and are hence very vulnerable to infections when exposed to the general population," says Laxminarayan. The most common source is the insanitary care of the umbilical cord. "With rising rates of drug-resistant bacteria in hospitals, they also pick up such germs. If such bacteria enter the blood, the chances of death are extremely high."
Killer germs multiply
Alarming snapshots are coming to the fore from across India: Neonates dying of ABR in the first four weeks of life; TB patients in metros not responding to any known antibiotics; rising ABR infections in hospitals; killer germs in tap water and drains in big cities; antibiotic contamination of rivers from pharma waste; use of antibiotics on livestock and crops that increases risk of resistance in humans; people without any history of disease showing inexplicable resistance to antibiotics in surveys.
Meera Syal, 60, had gone to her local hospital in west Delhi last year for a routine check-up after an asthma attack. She just had a mild wheezing, but the doctor insisted on hospital admission to check her airways. The next morning, however, the family found her on ventilator. She had pneumonia, they were told, and would be fine in a few days. Instead, over the next few days, her temperature spiked, leading to a seizure. She never recovered. She had picked up a deadly, drug-resistant form of pneumonia bacteria from the ventilator. "It's a rising menace in Indian hospitals and the consequences are critical," says Dr Randeep Guleria, professor, department of medicine at AIIMS, Delhi.
"This is an emergency no less than global warming, and calls for immediate redress," says microbiologist Dr Chand Wattal of Ganga Ram Hospital. Wattal and his colleagues studied 77,618 patients since 2002. The results show an alarming rise in ABR: Bacterium Klebsiella pneumoniae, which damages human lungs, stopped reacting to last-resort drugs carbapenems-from 2.4 per cent to 52 per cent in a decade.
Too casual about it
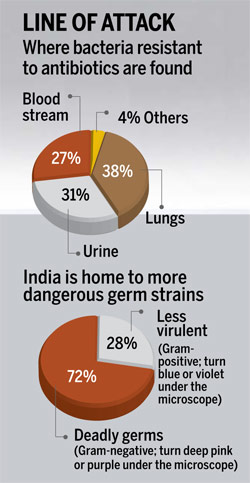
Click here to Enlarge
"Our attitude to antibiotics is too casual," says Dr K.S. Reddy, director of Public Health Foundation of India in Delhi. "They are cheap, easily available and can be picked up without prescription." Doctors grumble that patients stop coming to them if they don't prescribe antibiotics. A 2010 who survey reveals 53 per cent of Delhiites self-prescribe antibiotics; one in four skips the course once they feel better; and 18 per cent physicians prescribe antibiotics for common cold. The hard evidence came from Dr Anita Kotwani, pharmacologist with V.P. Chest Institute, Delhi University. Her 2011 study found that antibiotics form 39-43 per cent of drugs being sold in the city. Also, very powerful drugs, meant for hospital use, were being routinely dispensed, even for common infections. No wonder antibiotic consumption in India has gone up between 6 and 7 per cent annually since 2005. The fallout is worrying: In December 2012, for instance, amoxicillin-a standard formula for common cold in India-lost its efficacy, according to journal Lancet.
Wattal blames the lack of focus on ABR in medical curricula: "Most doctors prescribe antibiotics in a knee-jerk reaction to any infection, which may not even be needed." Doctors have to take responsibility, feels Dr Raja Dhar, chest physician at Fortis Hospital in Kolkata. The reason most patients develop resistance is injudicious use of antibiotics, incorrect regimens, inappropriate addition-deletion of drugs, lack of compliance with medications, he says. "And doctors play a crucial role in shaping patient mindsets."
Bad bugs, no drugs
New antibiotics can help stave off the catastrophe. But since 1987, no major antibiotic has been discovered. "The science of antibiotics is complex," says D.G. Shah, secretary-general of the Indian Pharmaceutical Alliance. One needs to find different ways of hitting the bacteria. Such research is expensive and time-consuming. "It's not profitable for global big pharma as antibiotics are for short-term use," he says. "Blockbuster drugs for chronic illnesses that people take every day for as long as they live are more profitable." At the root of the crisis is a "patent cliff", a term coined for the sheer number of major drugs coming off patent between 2010 and 2014. Patents protect the rights of original makers of a branded drug for 20 years to sell it exclusively. Once it expires, others can make and sell cheaper versions. "Loss of revenues is the biggest challenge to R&D innovation."
Are there measures we can take to make sure that the gains of modern medicine are not squandered? India needs an antibiotic policy and a national registry, inclusion of ABR in medical courses, monitoring of pharmacies so that antibiotics cannot be sold without prescription and ensuring infection-control protocols in hospitals. We are in a dangerous zone where life can end in any unexpected way: A nick from a shaving razor, a scrape from a fall, a rash from the swimming pool or a routine root canal. As Margaret Chan writes in the 2013 w.e.f report, "We're at the dawn of a post-antibiotic age."
Read more at:
Your Antibiotic is Sick: Bacteria are defying the most powerful medicines of all time. Is India ready for a world without antibiotics? : Cover Story - India Today